Saving Children through Xbox Cameras

The header image was purchased on Istock.com and is protected by copyright.
Children may suffer from respiratory failure due to lung infections. This can be difficult to predict by clinicians, whose analysis includes quantitative measurements (respiration rate) and qualitative observations (inhaled volume and chest indrawing). However, qualitative observation is difficult and imprecise when the volume is small, especially in infants. Researchers at the ÉTS Biomedical Information Processing Laboratory (LATIS), in collaboration with CHU Sainte-Justine, have designed a system to detect respiratory distress in children using 3D data recorded by a Microsoft KINECT camera system. Keywords: Breathing, Intensive Care, KINECT Camera, 3D Data, Surface Reconstruction.
Analyzing Respiratory Function
Analysis of respiratory function through visual examination is an important component in clinical evaluations. However, the accuracy of visual examinations is highly correlated to the clinician’s expertise [1,2]. There is currently no reliable method to quantitatively assess respiratory function in unventilated children. This is usually performed by visual examination and is therefore subjective. The purpose of our study is to standardize the assessment of respiratory failure. The main objective is to design and develop a computerized clinical decision support system (CCDSS) to detect respiratory failure in critically ill children (respiration rate, tidal volume, minute respiratory volume and thoraco-abdominal balancing [TAA]). The validation will be performed by comparing the respiratory status assessment by the CCDSS to the ventilator (gold standard).We believe that CDSS validation should have a potential to improve respiratory management especially during patient transportation when healthcare resources such as pediatric expert are limited.
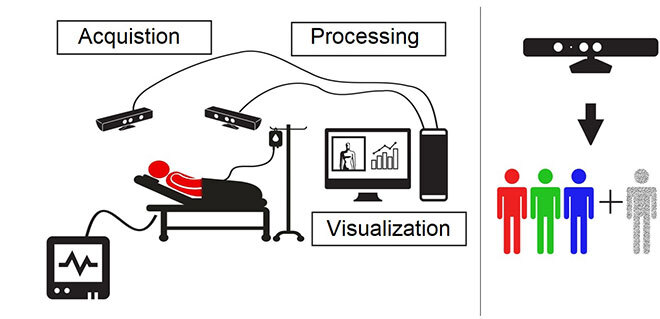
Figure 1—The CCDSS system calculating volume and respiration rate. The Xbox camera provides RGB (Red, Green, Blue) color information as well as the estimated depth for each pixel. These data are processed to perform a 3D reconstruction of the thoraco-abdominal surface.
Xbox Cameras in Intensive Care
We propose a new algorithm to calculate quantitative measures of respiration rate and tidal volume. Our technique is using recorded data from two Xbox cameras placed at two opposite corners of the patient’s bed. The objective of using two cameras is to maximize spatial coverage by recording breathing data of the thoraco-abdominal surface as well as of its lateral sides. The spatial organization, including cables and camera configurations, was optimized to facilitate the system deployment in intensive care units. Indeed, the camera system can easily be integrated in the patient’s bed. This configuration was tested and validated by the Sainte-Justine Hospital equipment inspection team.
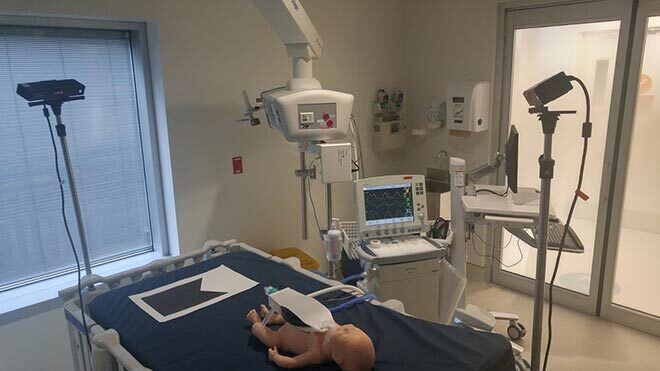
Figure 2—CCDSS setup in a critical care room
The first step is to align the two camera views in one single frame. A 2D marker was placed along a common line of sight of both cameras. Each camera estimates its relative position using the 2D marker.
The second step is to extract the breathing zones from the unified 3D view. This view, represented as a 3D point cloud, is first converted into a triangular mesh, from which the thoraco-abdominal surface is reconstructed [3]. Mesh discontinuities caused by the absence of chest wall back data are solved by adding a reference plane at a well-defined distance from the subject’s rib cage and its lateral parts.
Signal Generating Using Octree Encoding
The third step is to calculate a scalar value representing the extracted volume using recursive decomposition known as octree approach [4].Starting from a root node in the form of a single large cube, the octree is recursively subdivided into eight equal sized sub-cubes. This subdivision process continues until a predefined maximal depth is reached or if the new sub-regions are empty. The final volume is calculated for each frame by multiplying the number of remaining octrees by the size of a single unit.
Finally, a signal representing the volume variation of the reconstructed surface is calculated based on the previous steps. The signal frequency represents the patient’s respiration rate, while the amplitude variation indicates the inhaled volume [5].
Evaluating the Readings
The experiments were conducted in an intensive care room at Sainte-Justine Hospital in Montreal. The CCDSS was first tested by simulating breathing activity on a mannequin, designed according to neonatal anatomical and physiological characteristics, and then, tested on a real patient. Data were collected simultaneously from the CCDSS and a mechanical ventilator. Different air volumes corresponding to different age categories and weights (ranging from 10 ml to 500 ml) are delivered to the lungs by the ventilator to simulate breathing.
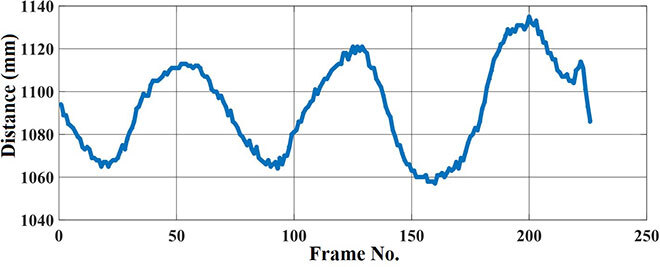
Figure 3—Depth variation of a torso area over 8 seconds (camera frequency: 30 frames per second)
Although results on the mannequin are slightly better, the CCDSS shows good accuracy and precision in calculating respiration rate and inhaled volume.
The system is an innovative and promising measurement tool intended to assist clinicians to monitor respiratory function. The experimental results show the robustness of the CCDSS in providing quantitative measurements of respiration, which will limit the evaluation subjectivity.
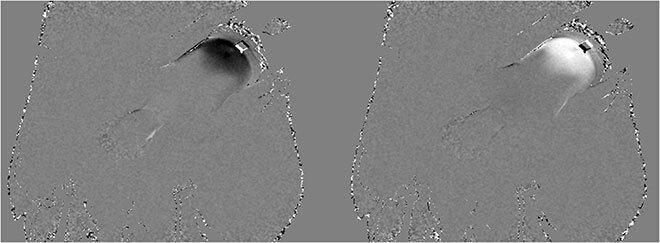
Figure 4—Breathing observation using the Xbox system: (a) on the left, inhaling, (b) on the right, exhaling. The white area indicates moving away from the camera (exhaling) and in black, approaching the camera (inhaling).
Conclusion
We proposed a 3D system to monitor children’s breathing in intensive care units. The system offers high spatial and temporal coverage of the thoraco-abdominal surface. Indeed, the system uses the complete information of breathing (3D data). The results yielded high accuracy and showed significant agreement with gold standard method. The system is a promising tool, helping caregivers in intensive care units. Our 3D imaging system offers an objective method to calculate the most relevant respiratory parameters in detecting respiratory distress.
Additional Information
Rehouma, H.; Noumeir, R.; Bouachir, W.; Jouvet, P.; Essouri, S. (2018). “3D imaging system for respiratory monitoring in pediatric intensive care environment”. Computerized Medical Imaging and Graphics, 70, 17–28.


