Optimizing Spinal Implants through Modeling

Fusion surgery is frequently used for treating scoliosis, fractures or spinal cord injury. Following fusion surgery, adjacent segments complications occur in up to 40% of the patients. Because of the high stiffness of the posterior instrumentations conventionally used, a stress concentration is created at the extremities of the implants, leading to adjacent segment complications. An innovative concept of shape memory alloys rods with variable flexural stiffness is proposed to lower the stress observed on the adjacent segments. Local Joule effect annealing was used to produce biocompatible rods with decreased proximal stiffness. The variable rods combined with transverse process hooks as upper anchors decrease the stress concentration at the adjacent segment and the pullout forces on the proximal anchors.
Introduction
With the increase in human life expectancy, the number of back-related problems continues to grow considerably. Commonly observed pathologies include scoliosis, problems of the lumbar spine, neurological injuries, and treatment-resistant pain. To alleviate these problems, some patients are required to undergo surgery (Deyo , Nachemson , and Mirza 2004). A common surgical approach includes spinal fusion surgery (arthrodesis), a procedure that joins two or more vertebrae to immobilize a spinal segment (Bederman et al. 2009). While this intervention offers the potential to reduce the patient’s discomfort significantly, it comes at the cost of a slight loss in spinal mobility. To achieve vertebral fusion, the orthopedic surgeon attaches rigid metal rods (made of titanium, cobalt-chromium alloys, or steel), to the vertebrae via pedicle screws. The efficiency of spinal fusion surgery has been proven and expresses itself through its high success rate (Fathy et al. 2010).
An important drawback of spinal fusion surgery originates from the large stiffness of the spinal implants. This stiffness can cause mechanical stress concentrations in the vertebral disc adjacent to the instrumentation (Figure 1), which can lead to complications, such as disc degeneration and fracture (DeWald and Stanley 2006; Park et al. 2004).
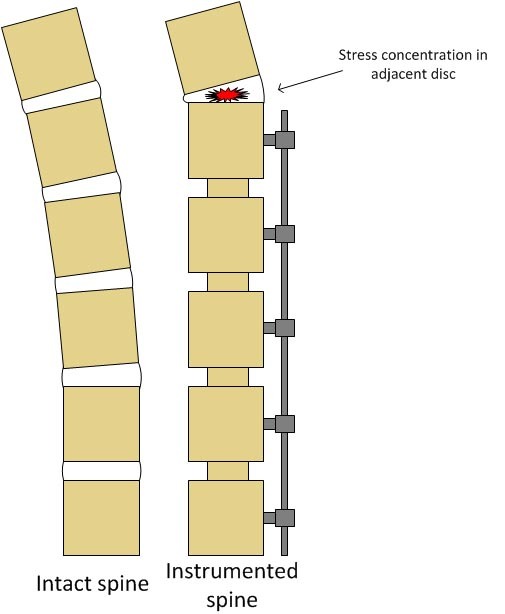
Figure 1 Comparison between an intact spine and a spine instrumented with spinal implants.
Project description
The present project represents a research collaboration between professor Vladimir Brailovski of the Shape Memory Alloys and Intelligent Systems Laboratory (LAMSI), professor Yvan Petit of the  Imaging and Orthopaedics research laboratory (LIO), both also affiliated with the Department of Mechanical Engineering of the École de technologie supérieure (ÉTS), and Dr. Jean-Marc Mac-Thiong, an orthopedic surgeon at the hôpital du Sacré-Cœur de Montréal. The objective of this collaboration is to develop spinal implants that can contribute to reduce adjacent disc disease subsequent to spinal fusion
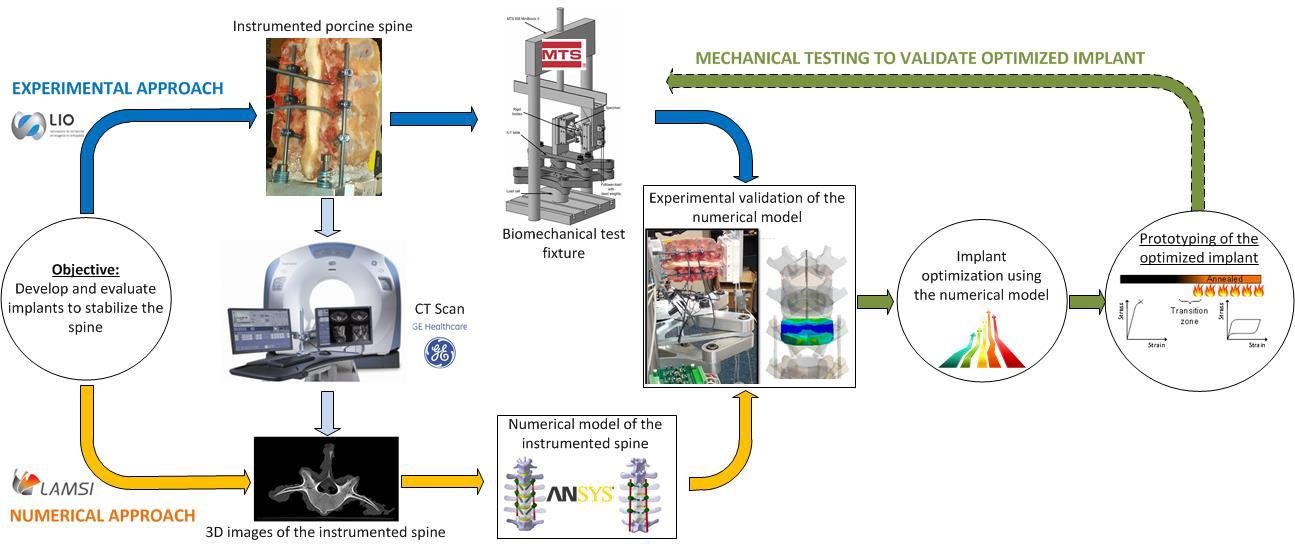
Imaging and Orthopaedics research laboratory (LIO), both also affiliated with the Department of Mechanical Engineering of the École de technologie supérieure (ÉTS), and Dr. Jean-Marc Mac-Thiong, an orthopedic surgeon at the hôpital du Sacré-Cœur de Montréal. The objective of this collaboration is to develop spinal implants that can contribute to reduce adjacent disc disease subsequent to spinal fusion  surgery. The project is conducted conjointly with Spinologics, a Montreal based medical technology company, and has led to the proposition of a new spinal implant (patent pending). The research objective is achieved using a mixed numerical and experimental approach (Figure 2). All numerical simulations are carried out at the ÉTS whereas the experimental work is performed at the hôpital du Sacré-Cœur de Montréal.
surgery. The project is conducted conjointly with Spinologics, a Montreal based medical technology company, and has led to the proposition of a new spinal implant (patent pending). The research objective is achieved using a mixed numerical and experimental approach (Figure 2). All numerical simulations are carried out at the ÉTS whereas the experimental work is performed at the hôpital du Sacré-Cœur de Montréal.
In vitro biomechanical tests are carried out on lumbar spine specimens of mature pigs. The biological specimens are dissected and instrumented with pedicle screws and spinal rods. Subsequently, the specimens are CT (Computed Tomography) scanned to obtain an image stack of the porcine lumbar spine. The images are processed to allow for an anatomically correct digital reconstruction of a given spinal segment and its instrumentation. Based on the reconstructed geometry, a finite element model is implemented which includes the vertebrae, the intervertebral discs, the spinal ligaments as well as the spinal instrumentation. Experimental measurements are carried out in parallel. Here, the specimen is subjected to various mechanical loading conditions to simulate common movements such as flexion, extension and lateral bending. Throughout these measurements, the movement of each vertebra is monitored using an infrared camera system. The pressure in the intervertebral discs that results from the different loading conditions is measured in the topmost disc of the instrumented spine as well as in the adjacent disc with the help of miniature pressure sensors. Furthermore, each pedicle screw is equipped with a strain gauge to monitor pullout forces and moments applied to them.
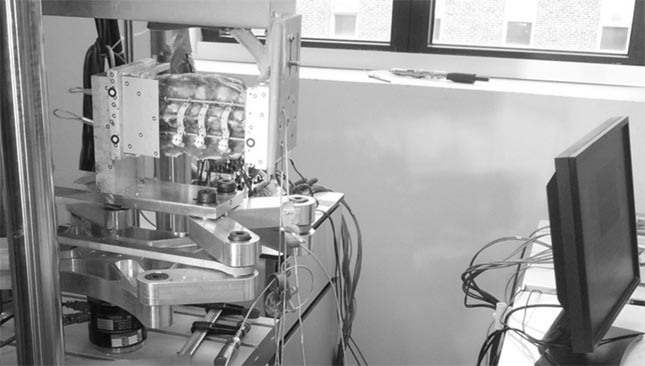
Figure 3 Test bench used for the experimental study
The numerical simulations are validated using the obtained experimental data in terms of the vertebral motion, intradiscal pressure, and the pullout force applied to the screws. Once validated, the numerical model provides a powerful tool that can be used to test new implants and to optimize the implant design in order to reduce adjacent disc disease. Upon identification of an optimized implant design, a physical prototype is manufactured and tested experimentally to verify the numerical results. This approach is carried out iteratively until both the numerical and experimental results lead to a reduced intradiscal pressure in the adjacent segment.
Areas of application
In the medical field, this work contributes to the development of implants which allow reducing the stress levels in the disc adjacent to the spinal instrumentation, thus contributing to alleviate adjacent disc disease, while providing adequate stability at the fusion site.
Additionally, a more general scientific value can be identified. The numerical tools developed in this project can be employed in future research projects that are related to studying the porcine lumbar spine and spinal instrumentations.
Concurrently, in combination with 3D printing (additive manufacturing techniques), the numerical model can be used to manufacture anatomically representative vertebrae that can serve for surgical planning and as a learning tool.
This project is an example of the close collaboration between École de technologie supérieure (ÉTS) and the Hôpital du Sacré-Cœur de Montréal, and it underlines the potential of a combined computational and experimental modeling approach for the development of complex biomedical devices..
.Funding
This project is funded by “le fonds de recherche du Québec – Nature et technologies” (FQRNT).