Planning the next generation of stents for congenital heart defects
The featured image was bought from Istock.com and is protected by copyright.
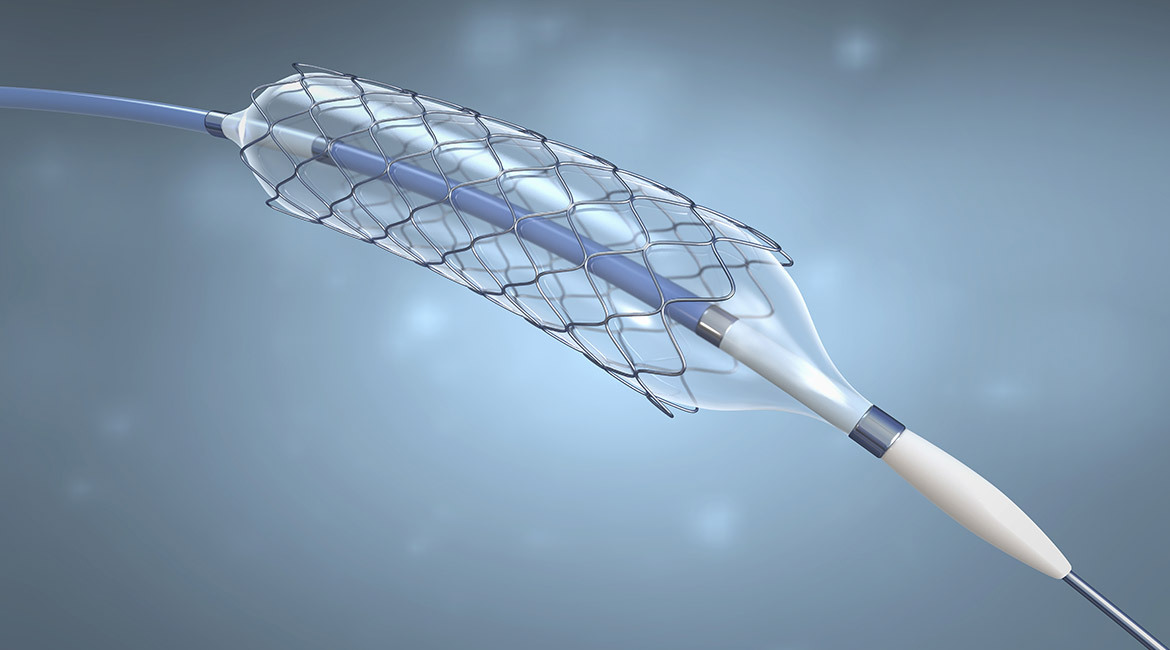
To facilitate stent planning in severe pulmonary artery stenosis a computational fluid dynamics simulation is run on patient specific geometries with two different stents By comparing the simulated hemodynamic parameters pressure and wall shear stress the suitability of the tested stent structures is assessed.
Pulmonary artery stenosis
Congenital heart disease affects 1% of births. Thanks to breakthroughs in the field, nearly 90% of children with congenital heart disease will reach adulthood, compared to 20% around the 1950s. One of these heart diseases, the stenosis of the pulmonary artery is a vessel narrowing that restricts blood flow. In severe cases it must be treated by catheterization. The procedure involves dilating the affected lesion with a balloon and, in some cases, placing a stent to maintain the artery structure. During the intervention the physician navigates the catheter using only 2 x-ray views. However, stenting requires a good evaluation of the diameter and length of the lesion. Visualization of the stenosis is sometimes difficult, given the complexity of the pulmonary arteries.
Simulation based on the patient specific geometry
The primary objective of this study is to determine the personalized geometry of the patient’s pulmonary arteries. The geometry is extracted from preoperative imaging acquired in CT or MRI. Secondly, our study optimizes the size and positioning of the stent based on fluid dynamics simulated from preoperative imaging. Finally, the biomechanical simulation model incorporates the pulsatility of arteries and the fluid dynamics simulation in the vessel. To do this, we used datasets from 16 patients, including pressure data acquired in vivo. The center line and geometry of the arteries are extracted from the data volume MRI and CT. Two types of stent are modeled: a conventional stent and a Y-shaped stent.
A software was developed to solve the Navier – Stokes equations and the Cauchy linear elastic equations using the stabilized finite element method. A linear solver with pre-dimensioning based on resistance is used. Blood is treated as a Newtonian fluid with constant viscosity. Our model is characterized by the possibility to simulate not only the geometry of the patient, but also the effect of the flow under the influence of the pulsatile movement. We validated this movement using data from the literature, as well as observations on angiographies. The movement representation could be the cornerstone to a better understanding of the stent interventions and also lead to a design really adapted to the patient’s anatomy.

Figure 1 Modeling steps of the pulmonary artery.
Comparison of simulated data with clinical data
Figure 2 illustrates the results of pressure gradients and shear stress difference at the artery wall for both stents, therewith showing the effect of the stent on the hemodynamic parameters. Pressure and shear stress were simulated because the pressure gradient and shear stress at the walls are good indicators of the severity of the stenosis. The simulation of the pressure is illustrated in the attached videos. Patient simulation is consistent with clinical observation. For patients P4, P7 and P8 no decrease in the gradient is observed, as predicted by the simulation. P14 already had a pressure gradient of zero before the procedure.

Figure 2 (a) Pressure gradient difference and time averaged wall shear stress difference for a regular stent and (b) with a Y-shaped stent
Conclusion
The use of CT and MRI preoperative imaging will one day assist clinicians and assess stenosis even before the intervention. Such simulation tools will lead to a better understanding of stenoses, through imaging and 3D modeling, better pre-intervention planning, and ultimately, improved patient care.
Additional information
For more information on this research, see the following article: Gundelwein L, Miró J, Barlatay FG, Lapierre C, Rohr K, Duong L. (2018). « Personalized stent design for congenital heart defects using pulsatile blood flow simulations » J Biomech. Vol 81. pp. 68-75.


